Nanoneedle breakthrough gives hope for cheaper cancer treatment
Media release
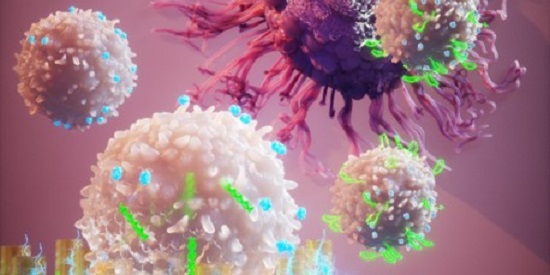
Australian scientists have successfully found a way to inject beneficial genetic material into white blood cells in a world-first breakthrough that could significantly improve treatment options for certain types of blood cancer.
A multidisciplinary team led by ARC Future Fellow Dr Roey Elnathan, from Deakin University's School of Medicine, and ARC Laureate Professor Nicolas Voelcker, from Monash University's Institute of Pharmaceutical Sciences (MIPS), has harnessed the power of nano-injection technology to improve outcomes in one of the world's newest forms of cancer immunotherapies, CAR-T cell therapy.
The researchers have published their preliminary findings in two high-impact journals, Advanced Materials and Materials Today
CAR-T cell therapy involves taking a cancer patient's white bloods cells (or 'T cells') and genetically engineering them before they are infused back into the patient to attack the cancer cells. Because of the number of steps involved, the process is slow and expensive, currently costing more than A$500,000 per patient.
Using tiny (nano)needles 100,000 times less than the width of a human hair, the research team has found a way to eliminate inactive viral vectors for genetically encoding the T cells. Viral vectors are commonly used to deliver genetic material into cells but result in costly treatment delays in current CAR-T cell manufacturing.
Dr Elnathan said there was an urgent need for a scalable, affordable, streamlined CAR-T cell manufacturing process that did not rely on viral vectors.
"We're using nanotechnologies to enable targeted delivery of advanced non-viral therapeutics into primary human immune cells, which are notoriously difficult to transfect," Dr Elnathan said.
"We have already shown that our nano-injection platform can re-engineer cells that benefit patients in vitro (in cell culture). We now need to test this technology at a clinical level."
Professor Voelcker said the research promises to change the business model of the CAR-T cell therapy – from boutique to widely affordable and the global market for the low-cost technology would be considerable.
"The non-viral process would reduce the complexities and eliminate the safety issues associated with viral vectors. And the nanotechnology has the potential to be conducted entirely within the hospital," Professor Voelcker said.
Deakin and Monash universities are collaborating with ULVAC Inc. in Japan to scale up fabrication of the nano-injection, which will be critical for scaling the new technology.
The research team, including Dr Crystal Chen and PhD student Ali-Resa Shokouhi from Monash University, is now benchmarking the efficiency in preclinical studies. The ARC Training Centre for Cell and Tissue Engineering Technologies is supporting researchers in the field of nanotechnology for emerging cancer immunotherapies.
Researchers anticipate it will take several years to test the technology in clinical settings before it becomes available as approved therapy.